Hammer Toe Cures
 Overview
Overview
Hammertoes are another forefoot deformity that can take a walker out of their activity. A hammertoe generally represent a tendon imbalance in the toes caused by one of the toe tendons getting an advantage over another toe tendon. Most commonly, it is one or all of the long extensor tendons on the top of the foot that gets an advantage over one or all of the flexor tendons Hammer toe on the bottom of the foot, to cause the first joint in the toe to be elevated above the ground. Most shoe wearing people chronically alter the delicate balance that co-exists amongst the toe tendons whether they know it or not.
Causes
Hammer toe is commonly caused by wearing shoes that are too narrow, tight or short on a regular basis. By doing so, your toe joints are forced into odd position. Over time, the tendons and muscles in your toe become shorter and cause it to bend. You can suffer a hammer toe if you have diabetes and the disease is worsening. If this occurs, you should contact your doctor right away. Arthritis can also cause hammer toes. Because your toe muscles get out of balance when you suffer from this joint disorder, tendons and joints of your toes are going to experience a lot of pressure.
 Symptoms
Symptoms
If the toes remain in the hammertoe position for long periods, the tendons on the top of the foot will tighten over time because they are not stretched to their full length. Eventually, the tendons shorten enough that the toe stays bent, even when shoes are not being worn. The symptoms of hammertoe include a curling toe, pain or discomfort in the toes and ball of the foot or the front of the leg, especially when toes are stretched downward, thickening of the skin above or below the affected toe with the formation of corns or calluses, difficulty finding shoes that fit well. In its early stages, hammertoe is not obvious. Frequently, hammertoe does not cause any symptoms except for the claw-like toe shape.
Diagnosis
Most health care professionals can diagnose hammertoe simply by examining your toes and feet. X-rays of the feet are not needed to diagnose hammertoe, but they may be useful to look for signs of some types of arthritis (such as rheumatoid arthritis) or other disorders that can cause hammertoe. If the deformed toe is very painful, your doctor may recommend that you have a fluid sample withdrawn from the joint with a needle so the fluid can be checked for signs of infection or gout (arthritis from crystal deposits).
Non Surgical Treatment
In many cases, conservative treatment consisting of physical therapy and new shoes with soft, spacious toe boxes is enough to resolve the condition, while in more severe or longstanding cases podiatric surgery may be necessary to correct the deformity. The patient's doctor may also prescribe some toe exercises that can be done at home to stretch and strengthen the muscles. For example, the individual can gently stretch the toes manually, or use the toes to pick things up off the floor. While watching television or reading, one can put a towel flat under the feet and use the toes to crumple it. The doctor can also prescribe a brace that pushes down on the toes to force them to stretch out their muscles.
Surgical Treatment
A variety of anaesthetic techniques are possible. Be sure an discuss this with your surgeon during your pre-op assessment. The type of surgery performed will depend on the problem with your toes and may involve releasing or lengthening tendons, putting joints back into place, straightening a toe and changing the shape of a bone.Your surgeon may fix the toes in place with wires or tiny screws.
What Is Hallux Valgus?
Overview
 The foot is made up of many small bones that sit perfectly together forming many joints. The big toe joint comprises of the first metatarsal and the proximal (close) phalanx of the toe. A bunion forms when base of the toe (first metatarsal) drifts away from the second metatarsal. The 1st metatarsal rotates and drops and so no longer sits in its correct alignment. The tip of the first toe then rotates and drifts inwards. Overtime, under the continuing stress of this altered position of the joint and the irritation that this causes, the joint can become inflamed.
The foot is made up of many small bones that sit perfectly together forming many joints. The big toe joint comprises of the first metatarsal and the proximal (close) phalanx of the toe. A bunion forms when base of the toe (first metatarsal) drifts away from the second metatarsal. The 1st metatarsal rotates and drops and so no longer sits in its correct alignment. The tip of the first toe then rotates and drifts inwards. Overtime, under the continuing stress of this altered position of the joint and the irritation that this causes, the joint can become inflamed.
Causes
What causes bunions? This question is often answered by blaming shoes. But in fact, shoes only play a small role in developing bunions. Yes, shoes, especially high heels cause abnormal squeezing of your forefoot. This in turn to help promote a bunion. But if everyone who wore high heels shoes had a bunion, there would be a lot more then the 15% prevalence we see in the general population. As you can see from the flow chart, genetics plays the major role in development of bunion deformities. Genetics determines the way your foot functions. Are you flatfooted? Are your joints flexible or stiff? Do you have a high arch? Do you have tight muscles? These traits are determined by your genetic code. These characteristics then govern how your bones and joints move when you walk. As an example, if your joints are very flexible, this can cause an abnormal amount of instability in your forefoot when you walk. Over time, this abnormal motion will cause the a bunion to develop by allowing your first metatarsal to "drift" towards the mid-line of your body.
Symptoms
Often the bunion is not painful and the individual leads a normal active life. Other times the bunion can be very painful, even debilitating. Pain is usually very achy and typically radiates to the toes and along the arch of the foot. Due to the abnormal positioning of the bones in the foot, sharp nerve pains could also be present.
Diagnosis
Generally, observation is adequate to diagnose a bunion, as the bump is obvious on the side of the foot or base of the big toe. However, your physician may order X-rays that will show the extent of the deformity of the foot.
Non Surgical Treatment
There are two ways to treat this pathological foot conditions, conservatively and surgically. Conservative treatment is the first line treatment which consists of splints and orthotic care to reduce the causative factors. Realigning the foot with the aid of an orthotic helps prevent further degeneration and/or reduce symptoms of HAV in any stage of its deformity. Along with orthotic care, patients may require debridement of corns and calluses produced due to extra forces produced on the foot. Orthotics will also help the function of the big toe joint as it allows it to bend in the correct position. Footwear advice is also essential in the conservative care of bunions, HAV, there may be a need to change footwear, so it is able to fit properly and be compliment with orthotics. Surgical correction of bunions, HAV is available, however should only be considered when conservative care has failed to reduce the onset of bunions, HAV. It is only considered if there is a clear sign that it will induce a better quality of life for the patient. 
Surgical Treatment
The aim of surgery is to correct the cause of the bunion and prevent it growing back. Which type of surgery your podiatric surgeon recommends will depend on the severity of your bunion. Because there are risks and complications with any type of surgery, it?s not usually advised unless your bunions are causing pain, or if it is starting to deform your other toes.
Prevention
To help prevent bunions, select your style and size of shoes wisely. Choose shoes with a wide toe area and a half-inch of space between the tip of your longest toe and the end of the shoe. Shoes also should conform to the shape of your feet without causing too much pressure.
What Actually Will Cause Feet To Over Pronate
Overpronation is by far the most common foot type. Pronation is not linked one-to-one with low arches. Although pronation lowers the arches, this does not mean that only those with low arches overpronate. People with high arches can also overpronate! Some of us have always overpronated, for others overpronation develops with age, weight gain, regular standing work or intensive exercise. Pronounced wear on the instep side of shoe heels can indicate overpronation, however it's best to get an accurate assessment.
Causes
Overpronation often occurs in people with flat feet, whose plantar fascia ligament is too flexible or too long, and therefore unable to properly support the longitudinal arch of the foot. People tend to inherit the foot structure that leads to overpronation. In a normal foot the bones are arranged so that two arches are formed, the longitudinal and the transverse. Ligaments hold all the bones in their correct positions, and tendons attach muscles to bones. If the bones are held together too loosely, they will tend to move inwards as this is the easiest direction for them to go. Over time the soft tissue structures will adjust to the misalignment and the foot will become permanently over-flexible, with a flat arch.
Symptoms
Common conditions seen with overpronation include heel pain or plantar fasciitis. Achilles tendonopathy. Hallus Valgus and/or bunions. Patellofemoral pain syndrome. Iliotibial band pain syndrome. Low back pain. Shin splints. Stress fractures in the foot or lower leg.
Diagnosis
Look at the wear on your shoes and especially running trainers; if you overpronate it's likely the inside of your shoe will be worn down (or seem crushed if they're soft shoes) from the extra strain.

Non Surgical Treatment
Your podiatrist will look at your current footwear to ensure that it is both well-fitted and possessed of adequate cushioning to protect your feet. Firm heel support is advised for over-pronators, and a good fit is important to ensure that the foot as a whole is well supported as instability can exacerbate the existing problems caused by over-pronation.
Surgical Treatment
Subtalar Arthroereisis. Primary benefit is that yje surgery is minimally invasive and fully reversible. the primary risk is a high chance of device displacement, generally not tolerated in adults.
An implant is pushed into the foot to block the excessive motion of the ankle bone. Generally only used in pediatric patients and in combination with other procedures, such as tendon lengthening. Reported removal rates vary from 38% - 100%, depending on manufacturer.
Severs Disease Physiotherapy
One of the most important things to know about Sever's disease is that, with proper care, the condition usually goes away within 2 weeks to 2 months and does not cause any problems later in life. Most children can return to physical activity without any trouble once the pain and other symptoms go away. The risk of recurrence goes away on its own when foot growth is complete and the growth plate has fused to the rest of the heel bone, usually around age 15.
Causes
Sever's disease can result from standing too long, which puts constant pressure on the heel. Poor-fitting shoes can contribute to the condition by not providing enough support or padding for the feet or by rubbing against the back of the heel. Although Sever's disease can occur in any child, these conditions increase the chances of it happening. Pronated foot (a foot that rolls in at the ankle when walking), which causes tightness and twisting of the Achilles tendon, thus increasing its pull on the heel's growth plate. Flat or high arch, which affects the angle of the heel within the foot, causing tightness and shortening of the Achilles tendon. Short leg syndrome (one leg is shorter than the other), which causes the foot on the short leg to bend downward to reach the ground, pulling on the Achilles tendon. Overweight or obesity, which puts weight-related pressure on the growth plate.
Symptoms
Athletes with Sever?s disease are typically aged 9 to 13 years and participate in running or jumping sports such as soccer, football, basketball, baseball, and gymnastics. The typical complaint is heel pain that develops slowly and occurs with activity. The pain is usually described like a bruise. There is rarely swelling or visible bruising. The pain is usually worse with running in cleats or shoes that have limited heel lift, cushion, and arch support. The pain usually goes away with rest and rarely occurs with low-impact sports such as bicycling, skating, or swimming.
Diagnosis
X-rays are normal in Sever's disease, but your doctor will probably get X-rays to rule out other problems. Treatment consists of non-steroidal anti-inflammatory medications and use of a heel lift to relieve tension on the calcaneal apophysis. In more severe cases, phycical therapy consisting of modalities to relieve the pain, and stretching exercises may be helpful. In extreme cases, castings have been used.
Non Surgical Treatment
Treatment aim is to lessen the load on the insertion of the Achilles tendon, along with pain relief if necessary. This can be achieved by modifying/reducing activity levels. Shoe inserts or heel raises. Calf stretches. Avoiding barefoot walking. Strapping or taping the foot to reduce movement. Orthotic therapy if due to biomechanical causes. Other treatment includes icing of the painful area to reduce swelling, pain medication if necessary and immobilisation of the affected limb in severe or long standing cases.
Recovery
The condition is normally self-limiting, and a return to normal activities is usually possible after a period of 2-3 months. In one study, all the patients treated with a physiotherapy programme (above) improved and could return to their sport of choice after two months of treatment. The condition may recur, although recurrence was uncommon, according to one study.
Posterior Tibial Tendon Dysfunction (PTTD)
Overview
Originally known as posterior tibial tendon dysfunction or insufficiency, adult-acquired flatfoot deformity encompasses a wide range of deformities. These deformities vary in location, severity, and rate of progression. Establishing a diagnosis as early as possible is one of the most important factors in treatment. Prompt early, aggressive nonsurgical management is important. A patient in whom such treatment fails should strongly consider surgical correction to avoid worsening of the deformity. In all four stages of deformity, the goal of surgery is to achieve proper alignment and maintain as much flexibility as possible in the foot and ankle complex. However, controversy remains as to how to manage flexible deformities, especially those that are severe. 
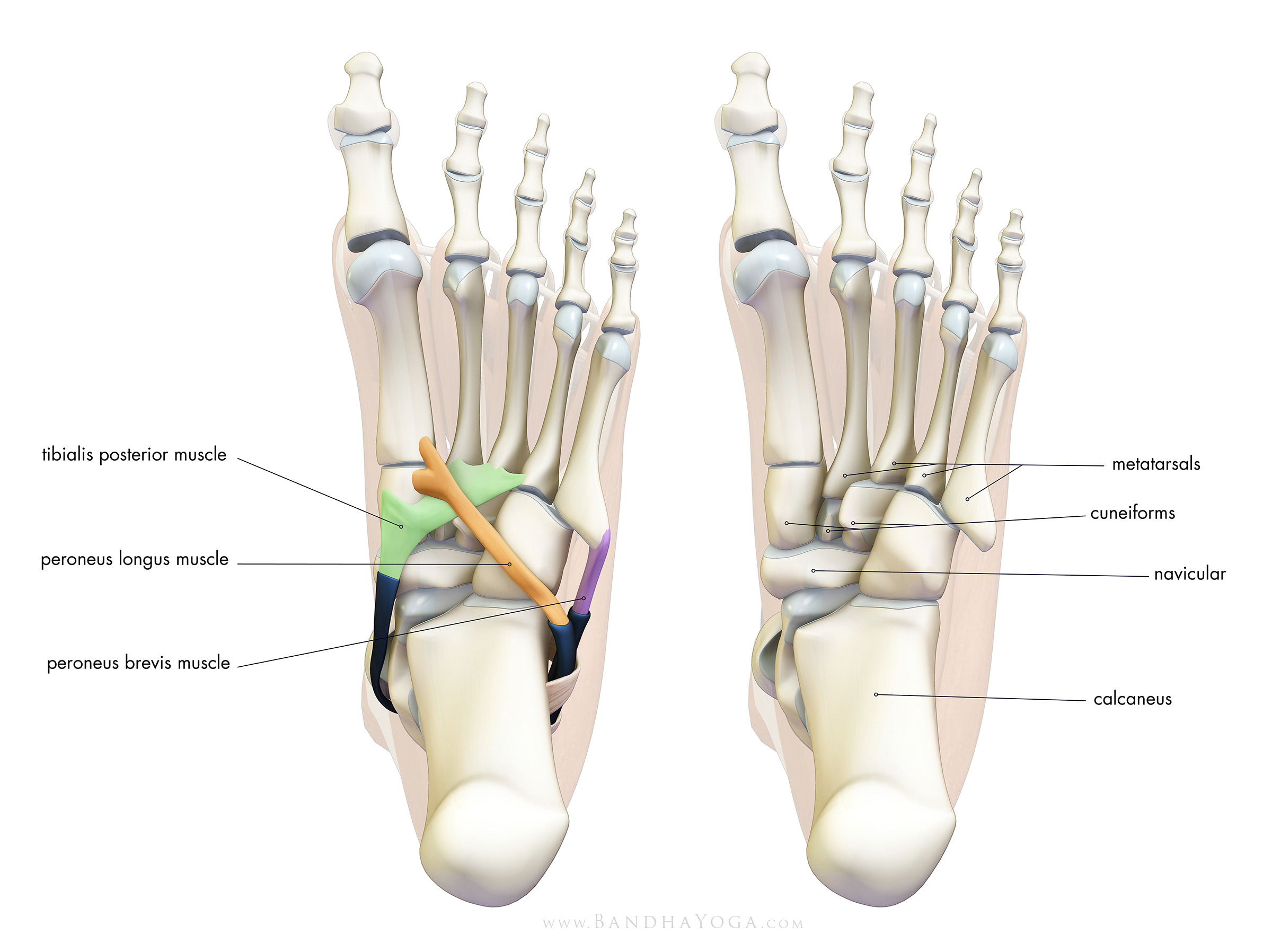
Causes
There are a number of theories as to why the tendon becomes inflamed and stops working. It may be related to the poor blood supply within the tendon. Increasing age, inflammatory arthritis, diabetes and obesity have been found to be causes.
Symptoms
The first stage represents inflammation and symptoms originating from an irritated posterior tibial tendon, which is still functional. Stage two is characterized by a change in the alignment of the foot noted on observation while standing (see above photos). The deformity is supple meaning the foot is freely movable and a ?normal? position can be restored by the examiner. Stage two is also associated with the inability to perform a single-leg heel rise. The third stage is dysfunction of the posterior tibial tendon is a flatfoot deformity that becomes stiff because of arthritis. Prolonged deformity causes irritation to the involved joints resulting in arthritis. The fourth phase is a flatfoot deformity either supple (stage two) or stiff (stage 3) with involvement of the ankle joint. This occurs when the deltoid ligament, the major supporting structure on the inside of the ankle, fails to provide support. The ankle becomes unstable and will demonstrate a tilted appearance on X-ray. Failure of the deltoid ligament results from an inward displacement of the weight bearing forces. When prolonged, this change can lead to ankle arthritis. The vast majority of patients with acquired adult flatfoot deformity are stage 2 by the time they seek treatment from a physician.
Diagnosis
Examination by your foot and ankle specialist can confirm the diagnosis for most patients. An ultrasound exam performed in the office setting can evaluate the status of the posterior tibial tendon, the tendon which is primarily responsible for supporting the arch structure of the foot.
Non surgical Treatment
Because of the progressive nature of PTTD, early treatment is critical. If treated soon enough, symptoms may resolve without the need for surgery and progression of the condition can be stopped. If left untreated, PTTD may create an extremely flat foot, painful arthritis in the foot and ankle, and will limit your ability to walk, run, and other activities. Your podiatrist may recommend one or more of these non-surgical treatments to manage your PTTD. Orthotic devices or bracing. To give your arch the support it needs, your foot and ankle surgeon may recommend an ankle brace or a custom orthotic device that fits into your shoe to support the arch. Immobilization. A short-leg cast or boot may be worn to immobilize the foot and allow the tendon to heal. Physical therapy. Ultrasound therapy and stretching exercises may help rehabilitate the tendon and muscle following immobilization. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Shoe modifications. Your foot and ankle surgeon may recommend changes in your footwear. 
Surgical Treatment
For those patients with PTTD that have severe deformity or have not improved with conservative treatments, surgery may be necessary to return them to daily activity. Surgery for PTTD may include repair of the diseased tendon and possible tendon transfer to a nearby healthy tendon, surgery on the surrounding bones or joints to prevent biomechanical abnormalities that may be a contributing factor or both.
Does Pain In The Arches Require Surgical Procedures ?
Plantar Fasciitis is a common condition that involves degenerative changes (wear and tear) of the thick fibrous band of tissue that runs from the heel bone beneath the arches through to the ball of the foot. Plantar Fasciitis can be caused by a range of factors including: high impact exercises, excessive body weight, hormonal changes and/or foot biomechanics (foot alignment with weight bearing including high arches or flat feet).

Causes
There are many different causes of flat feet, which can be separated into two main categories. The first category, congenital flat foot, is a condition that one is born with or is predisposed to at birth. This type includes the completely asymptomatic, pediatric flexible flat foot-by far the most common form of congenital flat foot. Flexible means that an arch is present until weight is put on the foot, at which time the arch disappears. This foot type is a result of the fact that all people are born with different physical features. Some people have bigger noses than others, just as some people have flatter feet (of course, there is no known correlation between the two). Any alteration in the many building blocks of the foot can influence its shape.
Symptoms
Symptoms of plantar fasciitis may occur anywhere along the arch, but it is most common near its attachment to the heel bone. Symptoms of plantar fasciitis vary, but the classic symptom is pain after rest--when you first get out of bed in the morning, or when you get up after sitting down for a while during the day. This is known as "post-static dyskinesia." The pain usually diminishes after a few minutes of walking, sometimes even disappearing, but the pain is commonly felt again the longer you're on the foot. Fasciitis can be aggravated by shoes that lack appropriate support, especially in the arch area, and by the chronic irritation of long-periods of standing, especially on concrete, and by being overweight. Other factors which influence this condition are gender (females get this more than men), age (30s to 50s are most common), and those with flatter-than-normal feet. It doesn't help that fascia doesn't heal particularly quickly. This is because it has relatively poor circulation, which is why it's white in colour.
Diagnosis
Magnetic Resonance Imaging (MRI) can show tendon injury and inflammation but cannot be relied on with 100% accuracy and confidence. The technique and skill of the radiologist in properly positioning the foot with the MRI beam are critical in demonstrating the sometimes obscure findings of tendon injury around the ankle. Magnetic Resonance Imaging (MRI) is expensive and is not necessary in most cases to diagnose posterior tibial tendon injury. Ultrasound has also been used in some cases to diagnose tendon injury, but this test again is usually not required to make the initial diagnosis.
Non Surgical Treatment
Cortisone, a type of steroid, is a powerful anti-inflammatory medication. It can be injected into the plantar fascia to reduce inflammation and pain. Your doctor may limit your injections. Multiple steroid injections can cause the plantar fascia to rupture (tear), which can lead to a flat foot and chronic pain. Supportive shoes and orthotics. Shoes with thick soles and extra cushioning can reduce pain with standing and walking. As you step and your heel strikes the ground, a significant amount of tension is placed on the fascia, which causes microtrauma (tiny tears in the tissue). A cushioned shoe or insert reduces this tension and the microtrauma that occurs with every step. Soft silicone heel pads are inexpensive and work by elevating and cushioning your heel. Pre-made or custom orthotics (shoe inserts) are also helpful. Most people sleep with their feet pointed down. This relaxes the plantar fascia and is one of the reasons for morning heel pain. A night splint stretches the plantar fascia while you sleep. Although it can be difficult to sleep with, a night splint is very effective and does not have to be used once the pain is gone. Your doctor may suggest that you work with a physical therapist on an exercise program that focuses on stretching your calf muscles and plantar fascia. In addition to exercises like the ones mentioned above, a physical therapy program may involve specialized ice treatments, massage, and medication to decrease inflammation around the plantar fascia. Extracorporeal shockwave therapy (ESWT). During this procedure, high-energy shockwave impulses stimulate the healing process in damaged plantar fascia tissue. ESWT has not shown consistent results and, therefore, is not commonly performed. ESWT is noninvasive-it does not require a surgical incision. Because of the minimal risk involved, ESWT is sometimes tried before surgery is considered.

Surgical Treatment
Surgery is considered only after 12 months of aggressive nonsurgical treatment. Gastrocnemius recession. This is a surgical lengthening of the calf (gastrocnemius) muscles. Because tight calf muscles place increased stress on the plantar fascia, this procedure is useful for patients who still have difficulty flexing their feet, despite a year of calf stretches. In gastrocnemius recession, one of the two muscles that make up the calf is lengthened to increase the motion of the ankle. The procedure can be performed with a traditional, open incision or with a smaller incision and an endoscope, an instrument that contains a small camera. Your doctor will discuss the procedure that best meets your needs. Complication rates for gastrocnemius recession are low, but can include nerve damage. Plantar fascia release. If you have a normal range of ankle motion and continued heel pain, your doctor may recommend a partial release procedure. During surgery, the plantar fascia ligament is partially cut to relieve tension in the tissue. If you have a large bone spur, it will be removed, as well. Although the surgery can be performed endoscopically, it is more difficult than with an open incision. In addition, endoscopy has a higher risk of nerve damage. The most common complications of release surgery include incomplete relief of pain and nerve damage. Most patients have good results from surgery. However, because surgery can result in chronic pain and dissatisfaction, it is recommended only after all nonsurgical measures have been exhausted.
Stretching Exercises
Point your toes. To ease foot pain and aching in your feet, lift one foot and roll it downward until the toes are pointed toward the ground. Then flex your foot. Repeat using the other foot. This exercise will help stretch out all the small muscles that are on the bottom of your feet, which can help relieve aching and improve blood circulation. Raise your heels. This exercise is good for relieving toe cramps caused by standing for hours in constricting shoes, says Kurtz. Bonus: It can also strengthen calf muscles and make them look more defined. Stand up and lift your heels so that you are standing on the balls of your feet. Hold for 10 seconds. Repeat 10 times. Squeeze your toes. To strengthen the toes and help alleviate foot pain from hammertoes (when a toe resembles a claw), separate your toes using corks or foam toe separators and then squeeze your toes together for five seconds. Repeat 10 times. Roll a ball. Want to create an instant massage for the bottom of your feet? Roll a golf ball or tennis ball under the ball of your foot. Apply light pressure for about two minutes. This exercise can be helpful for arch pain, cramps, and heel pain from plantar fasciitis. Stretch standing up. A weight-bearing, runners-type stretch can be helpful for foot pain in the arch. Stand up and place your toes against a wall; lean forward a little until you feel your arch stretch. Repeat using the other foot. Stretch sitting down. Sit barefoot and cross your left leg so that your ankle rests on your right thigh. Then hold your toes and bend them back toward your shin, stretching the band of tissue connecting the bottom of the heel to the ball. A University of Rochester study found that people living with plantar fasciitis had a 75 percent chance of having no pain within three to six months of performing this stretch three times daily. Give yourself a foot massage. Nothing spells pain relief like a good foot rub. Use the following technique recommended by Rhonda Crockett, a licensed massage therapist at Ohio State University?s Center for Integrative Medicine in Columbus. Start with your toes, using your thumb to massage them in circular motions. Then move to the arch under your foot and gradually work your way down to the heel, applying pressure with your fingers and palm of your hand. Use lotion to allow your hand to move smoothly over your foot. Relax in a warm bath with Epsom salts. The combination of warm water and Epsom salts will give you a double dose of pain relief and relaxation. Magnesium sulfate, the key compound in Epsom salts, has been found to relax muscles, reduce pain, and sedate the nervous system. Plus, warm water helps improve circulation in the feet and relieve muscle pain. Crockett recommends adding two cups of Epsom salts to a warm bath and soaking for 20 minutes.
What Is Posterior Tibial Tendon Dysfunction ?
Overview
Collapsed arches occur in five percent of adults 40 years and older, especially those who are overweight or maintain sedentary lifestyles. At the onset of the condition, adult acquired flatfoot can be controlled with anti-inflammatory medications, physical therapy, taping, bracing, and orthotics. While most cases of adult-onset flatfoot require surgery, congenital flatfoot is an entirely different condition that is best treated with orthotics in children. Ninety percent of children born with flat feet will be fine with conservative treatment. 
Causes
As the name suggests, adult-acquired flatfoot occurs once musculoskeletal maturity is reached, and it can present for a number of reasons, though one stands out among the others. While fractures, dislocations, tendon lacerations, and other such traumatic events do contribute to adult-acquired flatfoot as a significant lower extremity disorder, as mentioned above, damage to the posterior tibial tendon is most often at the heart of adult-acquired flatfoot. One study further elaborates on the matter by concluding that ?60% of patients [presenting with posterior tibial tendon damage and adult-acquired flatfoot] were obese or had diabetes mellitus, hypertension, previous surgery or trauma to the medial foot, or treatment with steroids?.
Symptoms
Initially, flatfoot deformity may not present with any symptoms. However, overtime as the tendon continues to function in an abnormal position, people with fallen arches will begin to have throbbing or sharp pain along the inside of the arch. Once the tendon and soft tissue around it elongates, there is no strengthening exercises or mechanism to shorten the tendon back to a normal position. Flatfoot can also occur in one or both feet. If the arch starts to slowly collapse in one foot and not the other, posterior tibial dysfunction (PTTD) is the most likely cause. People with flatfoot may only have pain with certain activities such as running or exercise in the early phase of PTTD. Pain may start from the arch and continue towards the inside part of the foot and ankle where the tendon courses from the leg. Redness, swelling and increased warmth may also occur. Later signs of PTTD include pain on the outside of the foot from the arch collapsing and impinging other joints. Arthritic symptoms such as painful, swollen joints in the foot and ankle may occur later as well due to the increased stress on the joints from working in an abnormal position for a long period of time.
Diagnosis
In the early stages of dysfunction of the posterior tibial tendon, most of the discomfort is located medially along the course of the tendon and the patient reports fatigue and aching on the plantar-medial aspect of the foot and ankle. Swelling is common if the dysfunction is associated with tenosynovitis. As dysfunction of the tendon progresses, maximum pain occurs laterally in the sinus tarsi because of impingement of the fibula against the calcaneus. With increasing deformity, patients report that the shape of the foot changes and that it becomes increasingly difficult to wear shoes. Many patients no longer report pain in the medial part of the foot and ankle after a complete rupture of the posterior tibial tendon has occurred; instead, the pain is located laterally. If a fixed deformity has not occurred, the patient may report that standing or walking with the hindfoot slightly inverted alleviates the lateral impingement and relieves the pain in the lateral part of the foot.
Non surgical Treatment
Conservative treatment is indicated for nearly all patients initially before surgical management is considered. The key factors in determining appropriate treatment are whether acute inflammation and whether the foot deformity is flexible or fixed. However, the ultimate treatment is often determined by the patients, most of whom are women aged 40 or older. Compliance can be a problem, especially in stages I and II. It helps to emphasise to the patients that tibialis posterior dysfunction is a progressive and chronic condition and that several fittings and a trial of several different orthoses or treatments are often needed before a tolerable treatment is found. 
Surgical Treatment
In cases of PTTD that have progressed substantially or have failed to improve with non-surgical treatment, surgery may be required. For some advanced cases, surgery may be the only option. Your foot and ankle surgeon will determine the best approach for you.